Understanding the Gray Area of Mammogram Results
October 08, 2025
October is Breast Cancer Awareness Month, a time when many women are reminded to schedule or follow up on their mammograms. These screenings are one of the most important tools we have for early detection, but the process can bring mixed emotions.
Getting called back after a mammogram can stir up fear, confusion, and frustration. Many women say the hardest part is not knowing what the results mean. But it’s important to remember it’s perfectly normal! Normally, 10-16% of mammograms performed will result in a call back. It is just a signal that something needs a closer look.
Here’s the important thing to remember: most mammogram findings are not cancer. But some results do signal the need for closer watching or extra care. Understanding this “gray area” can help you feel more informed.
When a Mammogram Isn’t “Normal” but Isn’t Cancer Either
Sometimes mammograms show changes that aren’t clearly dangerous but also aren’t completely typical.
- Benign findings: Harmless changes like cysts, fibroadenomas (smooth, rubbery lumps), or scattered calcifications. They may sound scary, but don’t increase your cancer risk.
- BI-RADS 0–3 results: Radiologists use a scoring system called BI-RADS:
- 0: More pictures needed
- 1: Normal or benign
- 3: "Probably benign,” almost always harmless, but checked again in 6 months to be safe
For many women, a callback ends up being just that: extra reassurance.
Atypical But Not Cancer: Hyperplasia
Sometimes, a biopsy shows breast cells that don’t look completely normal. This is called atypical hyperplasia. It’s not cancer, it’s not pre-cancer, and it doesn’t turn into cancer. But it does raise your lifetime risk of developing cancer compared to the normal population. Think of it as a yellow caution light, not an emergency, but a reason to watch more closely.
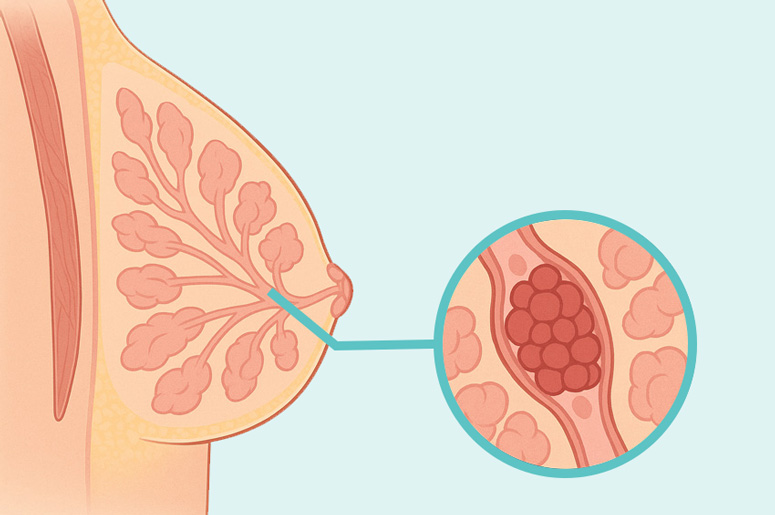
- ADH (atypical ductal hyperplasia): Abnormal cells in the milk ducts. Doctors may suggest closer monitoring and sometimes removing the small area for additional evaluation.
- ALH (atypical lobular hyperplasia): Abnormal cells in the lobules. Unlikely to require surgical evaluation, but still linked with a higher lifetime risk.
Most women with ADH or ALH never develop breast cancer (the risk is about 1-2% per year; that means there is a 98-99% chance of not developing cancer every year), but staying proactive is key.
High-Risk Conditions That Aren’t Invasive Cancer
Some diagnoses sit between benign changes and invasive breast cancer:
- LCIS (lobular carcinoma in situ): Similar to ALH, this is not cancer despite the name, but it is a marker of increased risk. Doctors may recommend more frequent screening.
- DCIS (ductal carcinoma in situ): A very early form of cancer that hasn’t spread (non-invasive). Highly treatable and often caught on routine screening.
These findings can sound frightening, but the silver lining is that they’re usually found early. That gives you and your care team time and choices.
What High-Risk Monitoring Looks Like
If you’re considered higher risk because of family history, genetic mutations (like BRCA), atypical hyperplasia, or LCIS, your doctor may suggest:
- More frequent imaging: Yearly mammograms plus breast MRI and/or ultrasound.
- Preventive medicine: Certain drugs can lower estrogen’s effect on the breast.
- Preventive surgery (rare): In select cases, very high-risk women may choose mastectomy. This is a personal decision, usually considered only with a strong family history or genetic mutations.
- Lifestyle steps: Staying active, maintaining a healthy weight, limiting alcohol, and not smoking.
Coping With the Waiting and the Worry
The hardest part is often the limbo between “not cancer” and “but we’ll keep watching.” You deserve both reassurance and clear information.
Ways to feel more in control:
- Ask for plain-language explanations. Don’t be afraid to say, “Can you explain that more simply?”
- Get a copy of your report. Knowing your BI-RADS score can ease anxiety.
- Consider a high-risk clinic. These clinics offer specialized monitoring and support.
- Connect with others. Support groups and online communities help many women feel less isolated in the waiting process.
Hope Lives Here
At Memorial Healthcare System, we believe early detection saves lives and prevention is just as important as treatment. That’s why we provide a full spectrum of breast health services to support women at every stage of care. From screening and diagnostic mammograms to high-risk monitoring and genetic testing and counseling, as well as breast cancer treatment and survivorship programs, Memorial offers care that is both compassionate and comprehensive.
Our nationally accredited Women’s Imaging Centers and Breast Cancer Center bring together expert radiologists, oncologists, surgeons, and nurse navigators who guide you every step of the way. Whether you need a routine screening, follow-up imaging, or specialized treatment, we are here to give you peace of mind and the best possible outcomes.
To schedule a mammogram, please call 855-530-2383 or visit our Mammogram page. Your health matters, and early action makes all the difference.

